Do-It-Yourself Contact Tracing Is a ‘Last Resort’ in Communities Besieged by Covid
Do-It-Yourself Contact Tracing Is a ‘Last Resort’ in Communities Besieged by Covid
By Brett Dahlberg, Kaiser Health News, January 8, 2021
The contact tracers of Washtenaw County in Michigan have been deluged with work and, to cope, the overburdened health department has a new tactic: It is asking residents who test positive for covid-19 to do their own contact tracing.
Washtenaw is a county of nearly 350,000 residents who live in and around the city of Ann Arbor, about 45 minutes from Detroit. Until mid-October, a county team of 15 contact tracers was managing the workload. But by Thanksgiving, more than 1,000 residents were testing positive for the coronavirus every week, and the tracers could not keep pace.
In Washtenaw County, the process starts with people called case investigators, who receive lab reports of positive coronavirus tests. Their job is to call anyone who has tested positive, tell them they need to isolate and ask them for the names of people with whom they have had close contact. After creating a list of potentially exposed “contacts,” investigators pass it to a new team to start the actual contact tracing. As the number of positive cases builds, the number of calls tracers must make swells.
But in recent weeks, it’s not just the number of positive cases that has increased, overwhelming the capacity of case investigators — so has the number of contacts that each infected person has, said contact tracer Madeline Bacolor.
“There’s just so many more people that are gathering and that are exposed,” she said. “It used to be, we had a case, and maybe that person had seen two people, and now it’s a whole classroom full of day care students or a whole workplace.”
The work to keep people who have been exposed to the virus away from people who have not is crucial, said public health professor Angela Beck, because it breaks viral transmission chains and prevents the virus from spreading unchecked through a community.
Beck teaches at the University of Michigan and runs the campus program for tracing coronavirus exposures among students.
When you’re trying to contain an infectious disease, she said, running out of contact tracers is “not a situation that you want to be in.”
But it’s happening now in health departments in Michigan and around the U.S. where contact tracing workforces have grown, but not fast enough to keep pace with the pandemic’s spread.
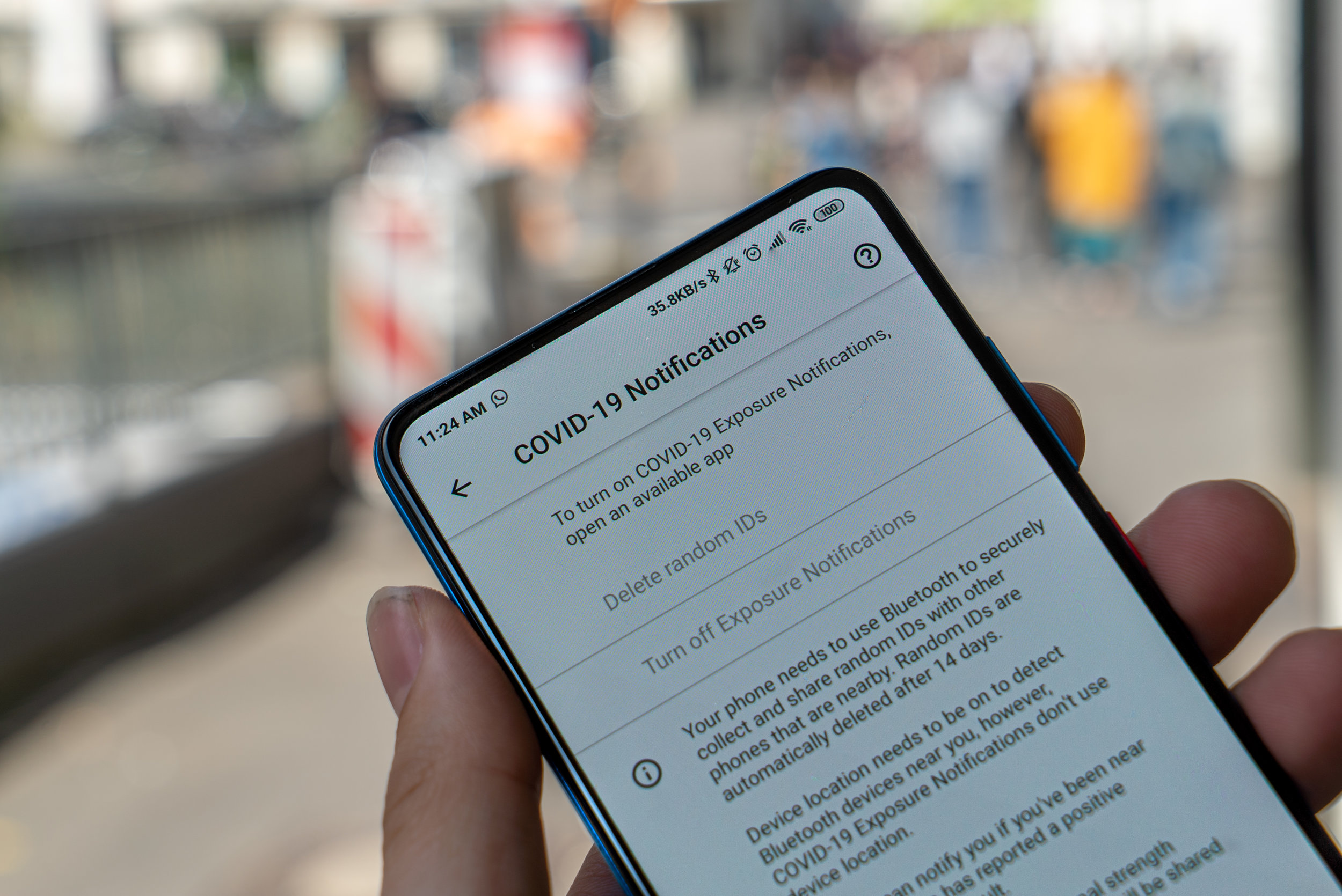
As a result, health departments are asking some residents with covid to reach out to their contacts on their own.
Trying ‘a Compromised Strategy’
Once billed as one of the fundamental tools for stemming the spread of the virus, contact tracing has fallen apart in many regions of the country. It’s a systematic breakdown that Lawrence Gostin, a professor of global health law at Georgetown University, said hasn’t happened since the spread and stigma of HIV and AIDS in the 1980s and ’90s.
In Michigan’s rural Upper Peninsula, a public health district spanning five counties warned residents that its tracers were overwhelmed and that they might not receive a call at all, despite testing positive. Health workers would need to focus their efforts on residents 65 and older, teens and children attending school in person, and people living in group settings.
In Michigan’s southwestern corner, contact tracers in Van Buren and Cass counties can no longer keep up with their calls. It’s the same situation in Berrien County: “If you test positive, take action immediately by isolating and notifying close contacts,” the county health officer urged residents in a press release.
Health officials have taken similar actions in all regions of the country, including Oregon, North Dakota, Ohio and Virginia.
Within many health departments, the shortage of contact tracers has been exacerbated by the communications challenge of relaying a recent change in quarantine guidance from the Centers for Disease Control and Prevention — it reduced the quarantine period from 14 days to 10 for some individuals exposed to the virus.
The idea behind the change was that the risk of transmission after 10 days of quarantine was low, and shorter quarantine periods might increase people’s willingness to comply with the orders. But the shift also meant that contact tracers had to spend time learning and explaining the new procedures just when caseloads were exploding.
“It makes things more confusing,” said Bacolor, the contact tracer in Washtenaw County. “People might be hearing something different from their job or school than they are from the health department.”
Asking infected people, some of whom might be sick, to call their own friends and families — in effect, conduct their own contact-tracing operation — is far from ideal, public health experts said.
“It is a last-resort tool,” said Beck, the University of Michigan professor. “It is the best that we can do in the situation that we’re in, but it’s a compromised strategy.”
Contact tracing is more than just alerting people to a potential exposure so they can quarantine. Part of the process is to conduct carefully structured interviews with those exposed, to determine if they’ve developed symptoms of covid-19. If so, contacts of those people also need to be traced and told to quarantine, to prevent the virus from proliferating through successive chains of people in the community.
Trained contact tracers also often ask valuable questions to learn more about how the virus was transmitted from person to person so that local health officials can piece together an understanding about which settings and activities seem particularly likely to promote spread — in-person choir rehearsals and crowded bars, for example — and which are unlikely to generate outbreaks.
Contact tracing is a key part of a tried-and-true strategy known as “test, trace and isolate.” Public health professor Beck said the strategy has been used all over the world and it works — when there are enough people and enough time to do it properly.
And she said effective contact tracing can help mitigate the economic pain of a pandemic because it means that only people with known exposures to the virus must stay away from workplaces and school and refrain from other activities.
But success requires significant investment in public health infrastructure, something that Beck and other researchers said has been lacking for decades in the U.S.
This story is part of a partnership that includes NPR and KHN.